Carbon monoxide (CO) is a colorless, odorless, and tasteless gas produced by the incomplete combustion of carbon-containing fuels such as gas, wood, coal, and petrol. Exposure can occur from car exhausts, house fires, faulty gas heaters, and industrial solvents containing methylene chloride, which is metabolized to CO in the body.
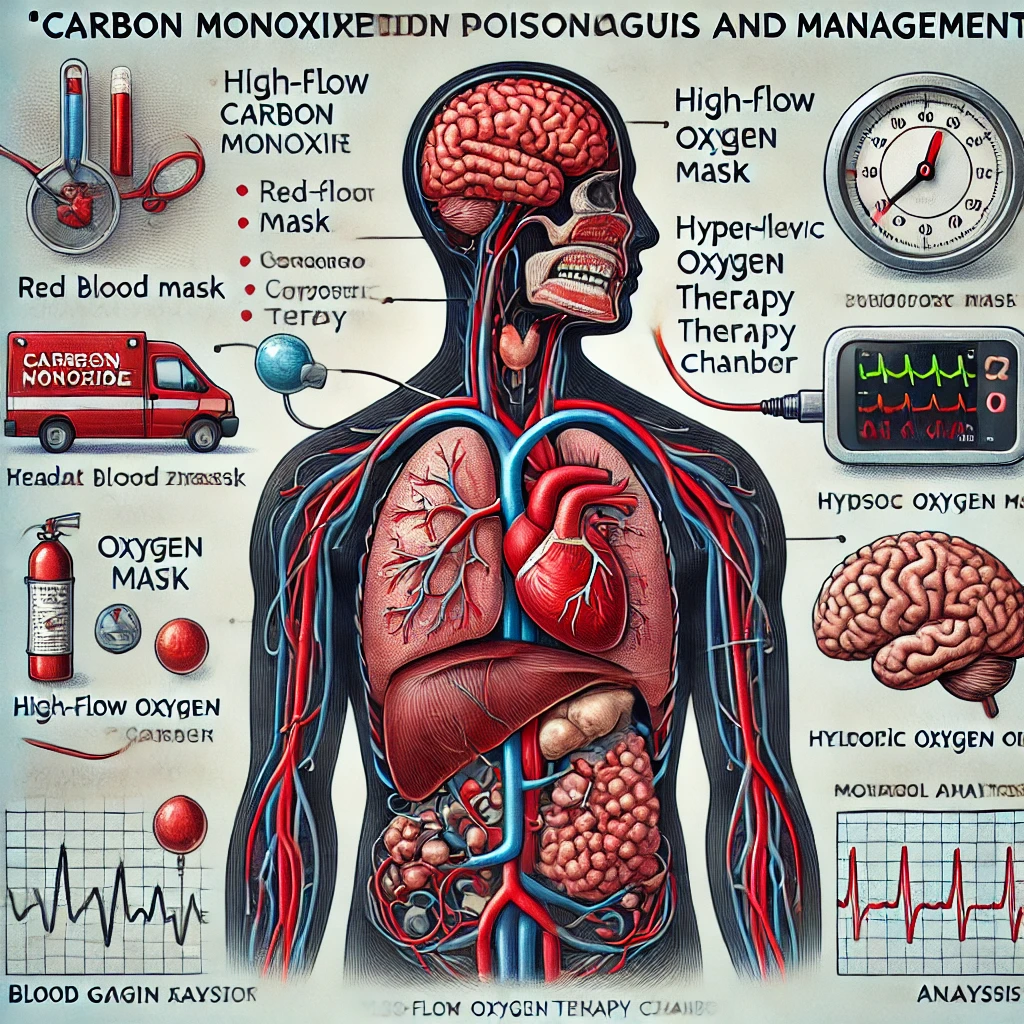
CO poisoning is a medical emergency due to its ability to bind haemoglobin (Hb), forming carboxyhaemoglobin (COHb), which reduces oxygen delivery to tissues, leading to severe hypoxia.
Pathophysiology
- CO binds to haemoglobin with 200-250 times the affinity of oxygen, forming COHb, which:
- Reduces oxygen transport.
- Impairs oxygen release to tissues.
- Leads to cellular hypoxia and metabolic acidosis.
- CO also binds to myoglobin and cytochrome enzymes, further impairing cellular respiration.
Clinical Features
Early Symptoms
- Headache
- Malaise
- Nausea and vomiting
- Dizziness
Severe Toxicity
- Neurological Symptoms:
- Confusion
- Seizures
- Loss of consciousness
- Coma with hyperventilation
- Cardiovascular Effects:
- Tachycardia
- Arrhythmias
- Myocardial ischemia
- Skin and Mucosa Appearance:
- Classically described as “cherry red” but often pink or normal
- May be cyanotic in hypoxic cases
- Hyperpyrexia (increased body temperature)
Diagnosis
1. Clinical Suspicion
- History of exposure (e.g., faulty heaters, house fires, enclosed spaces with fuel combustion).
- Consider in unexplained neurological or cardiovascular symptoms.
2. Laboratory Tests
- Arterial Blood Gas (ABG): May show metabolic acidosis.
- COHb Levels (Carboxyhaemoglobin):
- Normal: <3% (non-smokers), <10% (smokers)
- Mild poisoning: 10-20%
- Severe toxicity: >20%
- >40%: Risk of coma and death
- ECG & Troponins: Evaluate for myocardial ischemia.
- Lactate Levels: Increased due to tissue hypoxia.
Management
1. Immediate Actions
- Remove the patient from exposure.
- Ensure airway patency.
- Provide 100% high-flow oxygen using a non-rebreather mask.
- Intubate and provide mechanical ventilation if respiratory distress or coma is present.
2. Oxygen Therapy
- 100% Oxygen Therapy:
- Reduces COHb half-life from 4-6 hours to ~90 minutes.
- Continue until COHb <5% and symptoms resolve.
- Hyperbaric Oxygen Therapy (HBOT):
- Indications for HBOT:
- COHb >20-25%
- Neurological impairment (loss of consciousness, confusion, coma, seizures)
- Cardiovascular instability (arrhythmias, ischemia)
- Pregnant patients with COHb >15%
- Reduces COHb half-life to ~20 minutes.
- Conflicting evidence on long-term neurological benefits.
- Indications for HBOT:
3. Supportive Care
- Monitor cardiac function (ECG, troponins).
- Treat metabolic acidosis if present (e.g., sodium bicarbonate if severe).
- Manage seizures and arrhythmias accordingly.
Prevention
- Install and regularly check CO alarms.
- Ensure proper ventilation in homes using fuel-burning appliances.
- Avoid using generators or grills indoors.
- Routine inspection of gas heaters and fireplaces.
Conclusion
Carbon monoxide poisoning is a medical emergency requiring high clinical suspicion, prompt oxygen therapy, and potential hyperbaric oxygen treatment in severe cases. Prevention measures, such as CO detectors and regular maintenance of appliances, are key to reducing incidents.