1. Introduction to Stroke
A stroke is an acute neurological deficit caused by disruption of blood flow to the brain, leading to infarction (ischemic stroke) or hemorrhage (hemorrhagic stroke). Ischemic strokes account for about 80% of all strokes, while hemorrhagic strokes account for 20%.
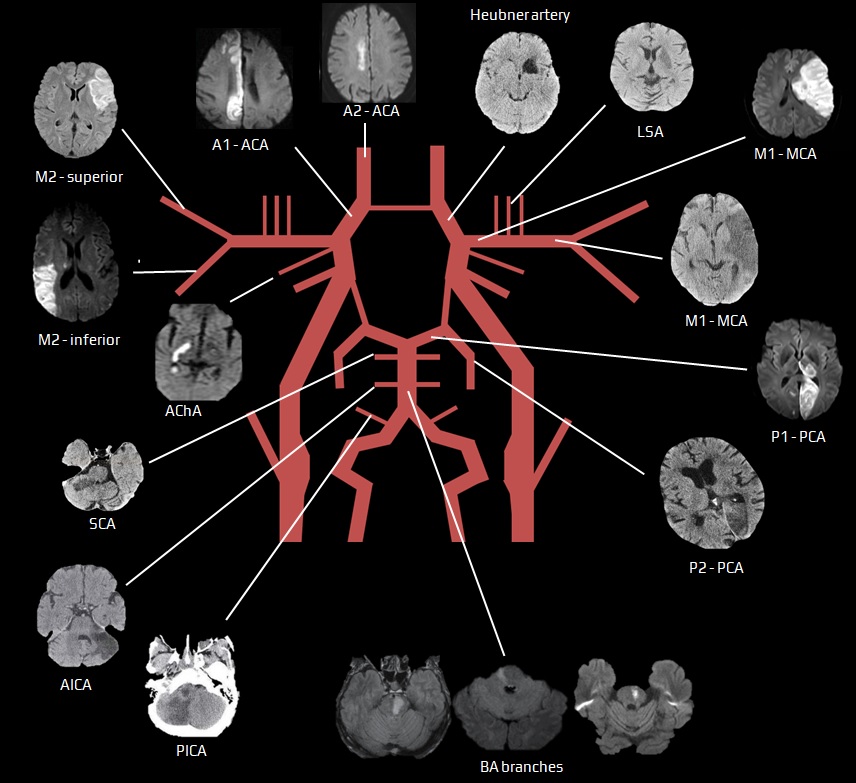
Understanding the vascular territories of the brain is essential for localizing strokes and predicting their clinical manifestations.
2. Classification of Stroke
(A) Ischemic Stroke (80%)
Caused by thrombosis, embolism, or systemic hypoperfusion, leading to brain infarction.
| Cause | Examples |
|---|---|
| Thrombotic | Atherosclerosis (large vessel disease), lacunar infarcts (small vessel disease) |
| Embolic | Cardioembolism (AF, endocarditis), carotid stenosis |
| Watershed (Hypoperfusion) | Severe hypotension (global ischemia) |
(B) Hemorrhagic Stroke (20%)
Caused by rupture of weakened blood vessels, leading to bleeding into the brain parenchyma or subarachnoid space.
| Type | Causes | Presentation |
|---|---|---|
| Intracerebral Hemorrhage (ICH) | Hypertension, amyloid angiopathy | Sudden severe headache, focal neuro deficits |
| Subarachnoid Hemorrhage (SAH) | Aneurysm rupture (Berry aneurysm) | Thunderclap headache, photophobia, nuchal rigidity |
3. Areas of Infarction in Stroke
Each major artery supplies a specific brain region, and stroke localization depends on identifying the affected vascular territory.
(A) Middle Cerebral Artery (MCA) Stroke (Most Common)
🔹 Supplies: Lateral frontal, temporal, and parietal lobes, basal ganglia, internal capsule
🔹 Clinical Features:
- Contralateral weakness & sensory loss (Face & upper limb > lower limb)
- Aphasia (if dominant hemisphere, usually left)
- Broca’s aphasia (expressive) – if frontal lobe affected
- Wernicke’s aphasia (receptive) – if temporal lobe affected
- Hemineglect (if non-dominant hemisphere, usually right)
- Homonymous hemianopia (loss of vision in the same side of both eyes)
| Feature | Dominant Hemisphere (Left MCA) | Non-Dominant Hemisphere (Right MCA) |
|---|---|---|
| Aphasia | Broca’s (if frontal), Wernicke’s (if temporal) | None |
| Hemineglect | None | Present |
| Motor & Sensory Loss | Right face & arm > leg | Left face & arm > leg |
(B) Anterior Cerebral Artery (ACA) Stroke
🔹 Supplies: Medial frontal and parietal lobes, anterior corpus callosum
🔹 Clinical Features:
- Contralateral weakness & sensory loss (Lower limb > Upper limb)
- Urinary incontinence (medial frontal lobe involvement)
- Apathy, personality changes, abulia (frontal lobe dysfunction)
- Alien hand syndrome (loss of voluntary hand movement control)
| Feature | Clinical Findings |
|---|---|
| Weakness & Sensory Loss | Contralateral leg > arm |
| Behavioral Changes | Apathy, abulia, emotional blunting |
| Other Signs | Urinary incontinence |
(C) Posterior Cerebral Artery (PCA) Stroke
🔹 Supplies: Occipital lobe, thalamus, hippocampus
🔹 Clinical Features:
- Contralateral homonymous hemianopia with macular sparing
- Memory impairment (temporal lobe, hippocampus involvement)
- Thalamic syndrome (Dejerine-Roussy syndrome – severe burning pain post-stroke)
- Alexia without agraphia (if dominant hemisphere)
| Feature | Clinical Findings |
|---|---|
| Vision Loss | Homonymous hemianopia (macular sparing) |
| Thalamic Syndrome | Contralateral pain & sensory loss |
| Memory Impairment | If temporal lobe affected |
(D) Lacunar Stroke (Small Vessel Disease)
🔹 Supplies: Deep brain structures (basal ganglia, thalamus, internal capsule, pons)
🔹 Common Syndromes:
- Pure Motor Stroke – Posterior limb of internal capsule (Contralateral hemiparesis)
- Pure Sensory Stroke – Thalamus (Contralateral sensory loss)
- Ataxic Hemiparesis – Pons/internal capsule (Weakness + ataxia)
| Lacunar Syndrome | Lesion Site | Clinical Features |
|---|---|---|
| Pure Motor Stroke | Internal capsule | Contralateral hemiparesis |
| Pure Sensory Stroke | Thalamus | Contralateral numbness, tingling |
| Ataxic Hemiparesis | Pons, internal capsule | Weakness + ataxia |
(E) Brainstem Stroke (Vertebrobasilar Territory)
🔹 Supplies: Brainstem (medulla, pons, midbrain), cerebellum
🔹 Clinical Features:
- Cranial nerve palsies (ipsilateral) + Contralateral hemiparesis
- Locked-in syndrome (bilateral pontine infarction)
- Vertigo, ataxia, nystagmus (if cerebellum involved)
| Stroke Syndrome | Affected Area | Clinical Features |
|---|---|---|
| Lateral Medullary (Wallenberg Syndrome) | Posterior Inferior Cerebellar Artery (PICA) | Ipsilateral Horner’s, dysphagia, ataxia |
| Medial Medullary Syndrome | Vertebral artery | Tongue deviation toward lesion, contralateral hemiparesis |
| Locked-In Syndrome | Bilateral pons | Quadriplegia, preserved consciousness |
4. Diagnostic Approach
| Test | Purpose |
|---|---|
| Non-contrast CT Brain | Rule out hemorrhage, detect large infarcts |
| MRI Brain (DWI sequence) | Best for early ischemic stroke detection |
| CT Angiography (CTA)/MR Angiography (MRA) | Assess vascular occlusion |
| Carotid Doppler | Evaluate carotid stenosis |
| ECG & Echocardiogram | Detect AF, cardioembolism |
5. Management of Stroke
(A) Acute Ischemic Stroke
🚨 Time = Brain!
- Thrombolysis (Alteplase/tPA) if within 4.5 hours
- Thrombectomy for large vessel occlusion
- Aspirin 300 mg (if outside thrombolysis window)
(B) Hemorrhagic Stroke
- Blood pressure control (IV labetalol, nicardipine)
- Surgical intervention if indicated (ICH evacuation, aneurysm clipping)
6. Key Takeaways
✅ MCA stroke → Face & arm > leg weakness, aphasia (dominant side), neglect (non-dominant)
✅ ACA stroke → Leg > arm weakness, behavioral changes, urinary incontinence
✅ PCA stroke → Homonymous hemianopia (macular sparing), thalamic pain syndrome
✅ Brainstem strokes → Cranial nerve deficits + crossed findings (ipsilateral face, contralateral body)
Would you like case-based scenarios or a diagnostic flowchart for rapid stroke assessment? 🚀