Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory condition characterized by airflow limitation that is not fully reversible. Acute exacerbation of COPD (AECOPD) is a sudden worsening of respiratory symptoms, requiring an immediate change in management. Exacerbations are associated with increased morbidity, hospitalizations, and mortality, making timely and effective treatment crucial.
This article provides a detailed approach to managing AECOPD using NICE (National Institute for Health and Care Excellence), British Thoracic Society (BTS), and Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.
Definition of AECOPD
An acute exacerbation of COPD is defined as a sustained worsening of baseline respiratory symptoms (dyspnea, cough, and/or sputum production) beyond normal day-to-day variation, leading to additional treatment.
Common Triggers
- Infections (viral or bacterial)
- Environmental factors (pollution, weather changes, smoke exposure)
- Non-adherence to COPD medication
- Pulmonary embolism (PE) (consider in sudden deterioration)
- Heart failure
Initial Assessment: A, B, C, D, E Approach
A structured ABCDE approach is critical in assessing the severity and guiding immediate interventions.
A – Airway
- Ensure patency of the airway.
- Assess for risk of aspiration (especially in altered consciousness due to CO₂ retention).
- Consider suctioning if excessive secretions are present.
B – Breathing
- Respiratory rate: Tachypnea is common.
- SpO₂ (Oxygen Saturation):
- Target 88-92% (higher O₂ can worsen hypercapnia).
- Use Venturi masks to provide controlled oxygen therapy.
- Auscultation:
- Wheezing → Bronchospasm
- Reduced breath sounds → Possible pneumothorax or severe obstruction
- Arterial Blood Gas (ABG) analysis:
- Type 2 respiratory failure: PaO₂ ↓, PaCO₂ ↑
- Acidosis (pH < 7.35): Indicates respiratory decompensation
- Consider non-invasive ventilation (NIV) if hypercapnia and acidosis persist.
C – Circulation
- Check BP, HR, ECG (tachycardia may indicate sepsis, PE, or hypoxia).
- Assess for signs of cor pulmonale (raised JVP, peripheral edema).
D – Disability (Neurological Status)
- Assess confusion or drowsiness (suggests CO₂ retention).
- Glasgow Coma Scale (GCS): If reduced, consider intubation.
E – Exposure
- Look for cyanosis, accessory muscle use, or cachexia.
- Check temperature (infection assessment).
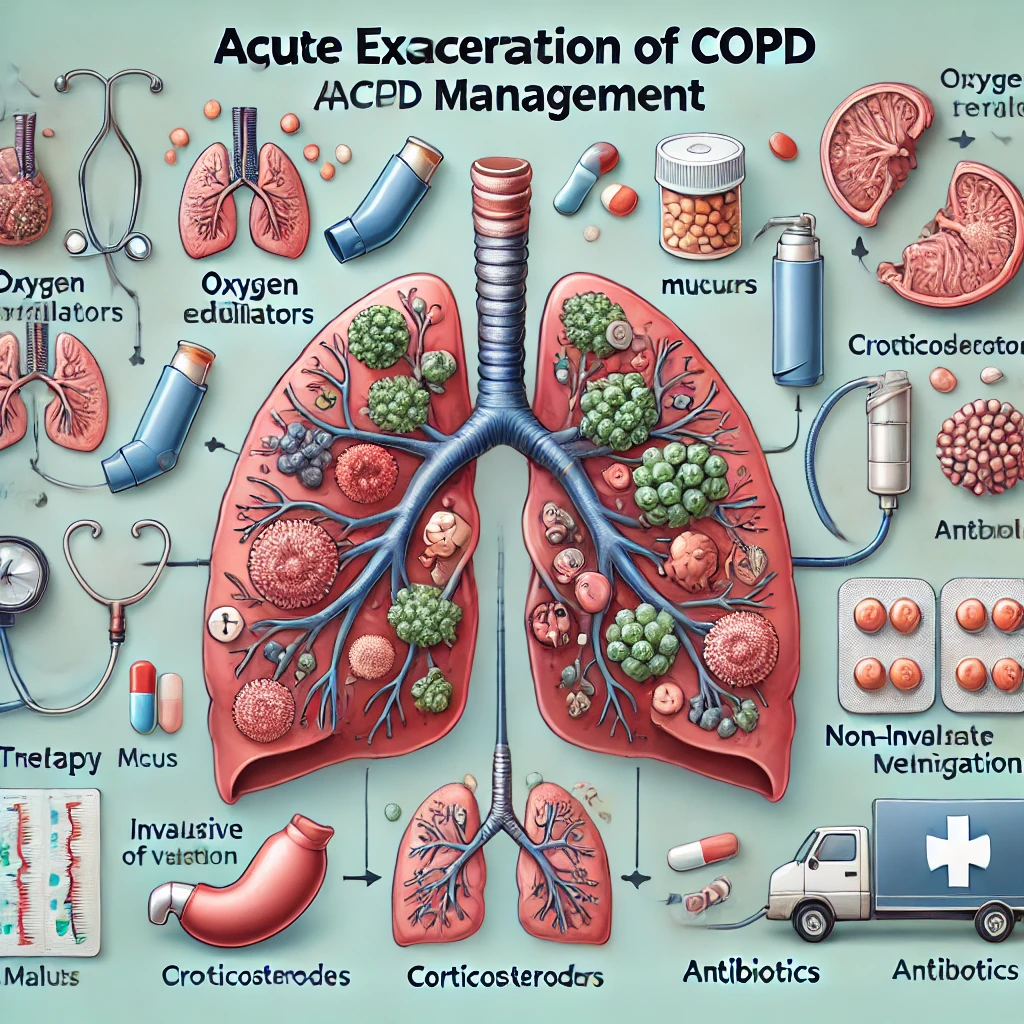
Management of AECOPD
1. Controlled Oxygen Therapy
- Target SpO₂: 88-92%.
- Start with 24-28% Venturi mask.
- Avoid excessive oxygenation (risk of CO₂ retention and worsening acidosis).
2. Bronchodilator Therapy
Short-acting beta-agonists (SABAs) and antimuscarinics
- Salbutamol 2.5-5 mg nebulized every 20-30 mins or via inhaler (MDI with spacer).
- Ipratropium bromide 500 mcg nebulized every 4-6 hours.
- Consider combination nebulization (Salbutamol + Ipratropium) for severe cases.
3. Corticosteroids
- Prednisolone 30-40 mg PO daily for 5 days.
- No need for tapering if <3 weeks use.
- IV Hydrocortisone (100 mg 6-hourly) if oral steroids not feasible.
4. Antibiotics (If Indicated)
- Consider if sputum is purulent or there is evidence of pneumonia.
- Empirical choices (as per NICE & BTS guidelines):
- Amoxicillin 500 mg TDS
- Doxycycline 200 mg stat, then 100 mg OD
- Clarithromycin 500 mg BD
- Adjust based on sputum culture results.
5. Non-Invasive Ventilation (NIV) – Indications
- pH < 7.35 and PaCO₂ > 6.5 kPa despite medical therapy.
- Severe respiratory distress with hypercapnia.
- Type 2 respiratory failure with acidosis.
6. Mechanical Ventilation – Indications
- Failure of NIV or worsening ABG values.
- Impending respiratory arrest.
- Severe hemodynamic instability.
Criteria for Hospital Admission
Admit if:
- Severe dyspnea not improving with initial treatment.
- Persistent hypoxia (SpO₂ < 88%) or worsening hypercapnia.
- Acute confusion or reduced GCS.
- Hemodynamic instability.
- Recurrent exacerbations requiring frequent intervention.
Discharge Planning & Long-Term Management
Criteria for Safe Discharge
- Stable respiratory status (SpO₂ ≥ 90% on minimal O₂).
- No worsening acidosis or CO₂ retention.
- Mobilizing independently.
- Supportive home environment and follow-up arranged.
Preventing Future Exacerbations
- Smoking cessation (most effective intervention for disease progression).
- Optimized maintenance therapy:
- Long-acting bronchodilators (LAMA/LABA)
- Inhaled corticosteroids (ICS) if indicated
- Vaccination (Influenza, Pneumococcal)
- Pulmonary rehabilitation
- Self-management plan (Recognizing early signs of exacerbation and when to seek help).
Conclusion
Acute exacerbations of COPD require a systematic approach to ensure timely and effective management. Early recognition, appropriate oxygen therapy, bronchodilators, corticosteroids, and NIV if necessary can significantly reduce mortality and improve patient outcomes. Preventative strategies such as smoking cessation, vaccination, and pulmonary rehabilitation are crucial in reducing the frequency of exacerbations.
For ongoing management, adherence to NICE, BTS, and GOLD guidelines ensures best practice and improved patient quality of life.