The brachial plexus is a vital nerve network supplying the upper limb, frequently encountered in clinical practice due to its involvement in trauma, nerve compression syndromes, and surgical procedures. A thorough understanding of its anatomy, function, and injury patterns is crucial for accurate diagnosis and management.
1. Anatomy of the Brachial Plexus
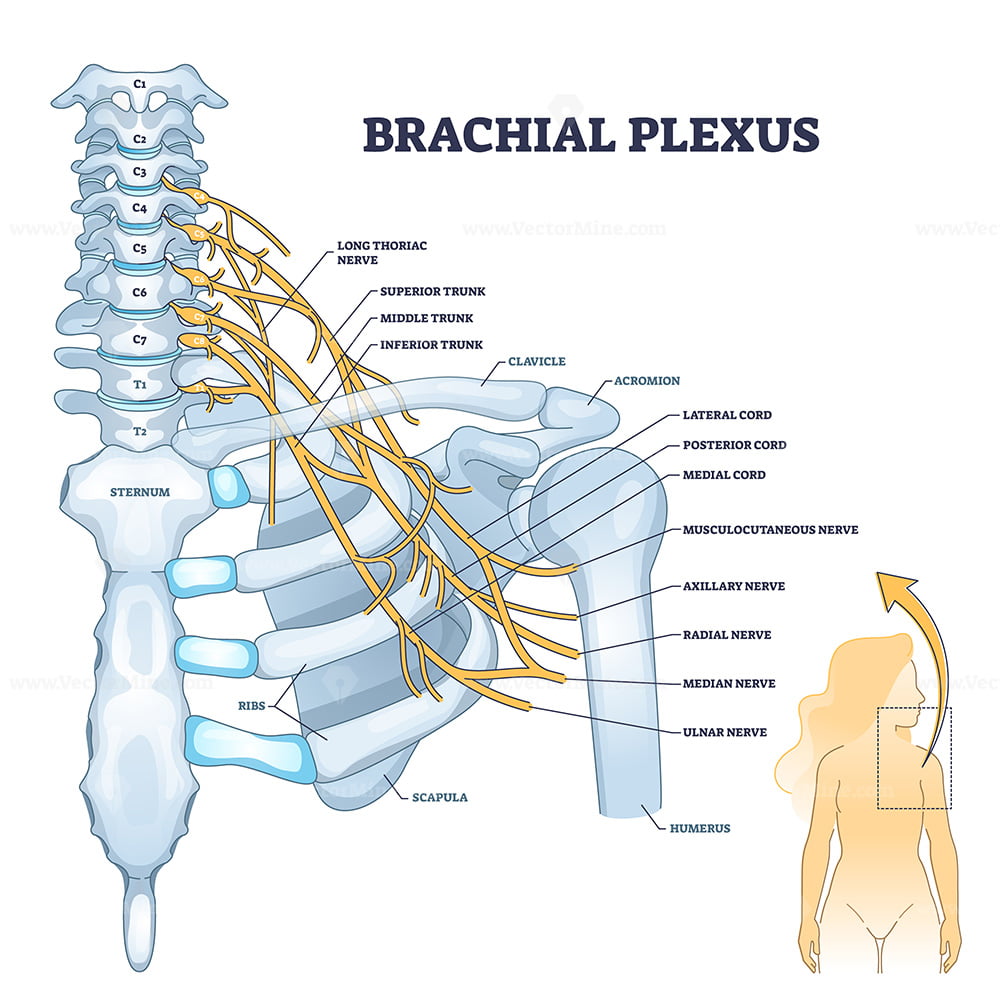
The brachial plexus originates from the ventral rami of C5-T1 and extends from the neck into the axilla, providing motor and sensory innervation to the upper limb.
Structural Organization (Mnemonic: Remember To Drink Cold Beer)
The plexus is systematically divided into five regions:
| Part | Mnemonic | Details |
|---|---|---|
| Roots | Remember | C5, C6, C7, C8, T1 (ventral rami) |
| Trunks | To | Superior (C5-C6), Middle (C7), Inferior (C8-T1) |
| Divisions | Drink | Each trunk divides into anterior and posterior divisions |
| Cords | Cold | Lateral, Medial, Posterior (relative to the axillary artery) |
| Branches | Beer | Five major terminal branches (see below) |
Major Branches and Their Functions
| Branch | Roots | Muscles Supplied | Key Functions |
|---|---|---|---|
| Musculocutaneous | C5-C7 | Biceps brachii, Brachialis, Coracobrachialis | Elbow flexion, Forearm supination |
| Axillary | C5-C6 | Deltoid, Teres minor | Shoulder abduction (15-90°) |
| Radial | C5-T1 | Triceps, Extensors of wrist & fingers | Elbow, wrist, and finger extension |
| Median | C5-T1 | Most forearm flexors, Thenar muscles | Wrist & finger flexion, Thumb opposition |
| Ulnar | C8-T1 | Intrinsic hand muscles, FCU, FDP (medial) | Fine finger movements, Grip strength |
2. Clinical Correlations & Nerve Injuries
Brachial plexus injuries can arise from trauma, obstetric complications, or nerve compression syndromes. Understanding the characteristic deficits aids in diagnosis and management.
(A) Upper Brachial Plexus Injury (Erb’s Palsy – “Waiter’s Tip”)
- Cause: Injury to C5-C6 roots due to excessive lateral traction on the neck
- Common scenarios: Birth trauma (shoulder dystocia), fall on the shoulder, motorcycle accidents
- Deficits:
- Arm adducted (Deltoid paralysis – Axillary nerve)
- Arm medially rotated (Infraspinatus paralysis – Suprascapular nerve)
- Elbow extended, forearm pronated (Biceps paralysis – Musculocutaneous nerve)
- Clinical Sign: “Waiter’s Tip” position
- Management:
- Supportive therapy (physiotherapy, splinting)
- In severe cases, nerve grafting may be considered
(B) Lower Brachial Plexus Injury (Klumpke’s Palsy – “Claw Hand”)
- Cause: Injury to C8-T1 roots, often due to excessive arm abduction
- Common scenarios: Traction injury during birth, grabbing a falling object
- Deficits:
- Intrinsic hand muscle weakness (affecting both ulnar and median nerve functions)
- Claw hand deformity (hyperextension of MCP, flexion of PIP/DIP joints)
- Management:
- Splinting to improve function
- Occupational therapy for hand function rehabilitation
(C) Radial Nerve Injury (“Wrist Drop”)
- Common Causes:
- Midshaft humeral fractures (direct trauma)
- Prolonged compression (Saturday night palsy)
- Improper use of crutches
- Deficits:
- Wrist drop (loss of wrist and finger extension)
- Weak grip strength
- Loss of sensation over dorsal hand (thumb and index web space)
- Management:
- Nerve conduction studies (NCS/EMG) for prognosis
- Splinting & physiotherapy
- Surgical decompression if persistent
(D) Ulnar Nerve Injury (“Ulnar Claw”)
- Common Causes:
- Medial epicondyle fracture (elbow region)
- Compression at Guyon’s canal (cyclist’s palsy)
- Deficits:
- Clawing of 4th & 5th fingers (Hyperextension at MCP, flexion at IP joints)
- Weak grip strength (loss of intrinsic hand muscles)
- Sensory loss over medial hand (ulnar distribution)
- Management:
- Splinting & physiotherapy
- Surgical decompression in severe cases
(E) Median Nerve Injury (“Hand of Benediction”)
- Common Causes:
- Supracondylar fracture of humerus
- Carpal tunnel syndrome (compression at wrist level)
- Deficits:
- Loss of thumb opposition (Thenar atrophy)
- “Hand of Benediction” when attempting a fist (due to loss of flexion in lateral digits)
- Management:
- Wrist splinting
- Carpal tunnel release if compression is the cause
3. Diagnostic Approach
A stepwise approach is essential for diagnosing brachial plexus injuries.
(A) Clinical Examination
- Motor testing for weakness patterns
- Sensory mapping to identify affected dermatomes
- Reflexes:
- Absent biceps reflex (C5-C6) → Suggests Erb’s palsy
- Absent triceps reflex (C7) → Suggests radial nerve involvement
(B) Investigations
| Test | Use |
|---|---|
| Electromyography (EMG) | Identifies nerve conduction defects |
| MRI Brachial Plexus | Best for visualizing nerve root injuries |
| Nerve Conduction Studies (NCS) | Assesses functional deficits |
4. Management Strategies
(A) Conservative Management
- Physical therapy to maintain range of motion
- Splinting to prevent contractures
- Pain management (neuropathic pain often requires gabapentinoids)
(B) Surgical Interventions
- Nerve grafting or transfers in severe injuries
- Decompression surgeries for entrapment neuropathies
5. Key Takeaways
✅ Brachial plexus lesions present with characteristic motor and sensory deficits.
✅ Understanding nerve root involvement helps in accurate diagnosis.
✅ Early physiotherapy and splinting can improve long-term outcomes.
✅ Surgical intervention is reserved for severe or refractory cases.
Further Reading
- NHS Brachial Plexus Injury Overview: NHS UK
- NICE Guidelines on Peripheral Nerve Injuries: NICE Guidelines