A hernia is the abnormal protrusion of an organ or tissue through a defect in the surrounding structures that usually contain it. This commonly occurs in the abdominal wall, involving the intestines or other intra-abdominal contents. Understanding hernia anatomy, classification, and clinical implications is essential for accurate diagnosis and management.
1. Basic Anatomy of a Hernia
A hernia consists of three main components:
| Component | Description |
|---|---|
| Hernial Sac | The peritoneal outpouching containing the herniated contents. |
| Hernial Ring | The defect in the fascia or muscle through which the contents protrude. |
| Hernial Contents | May include bowel, omentum, or other intra-abdominal structures. |
2. Classification of Hernias
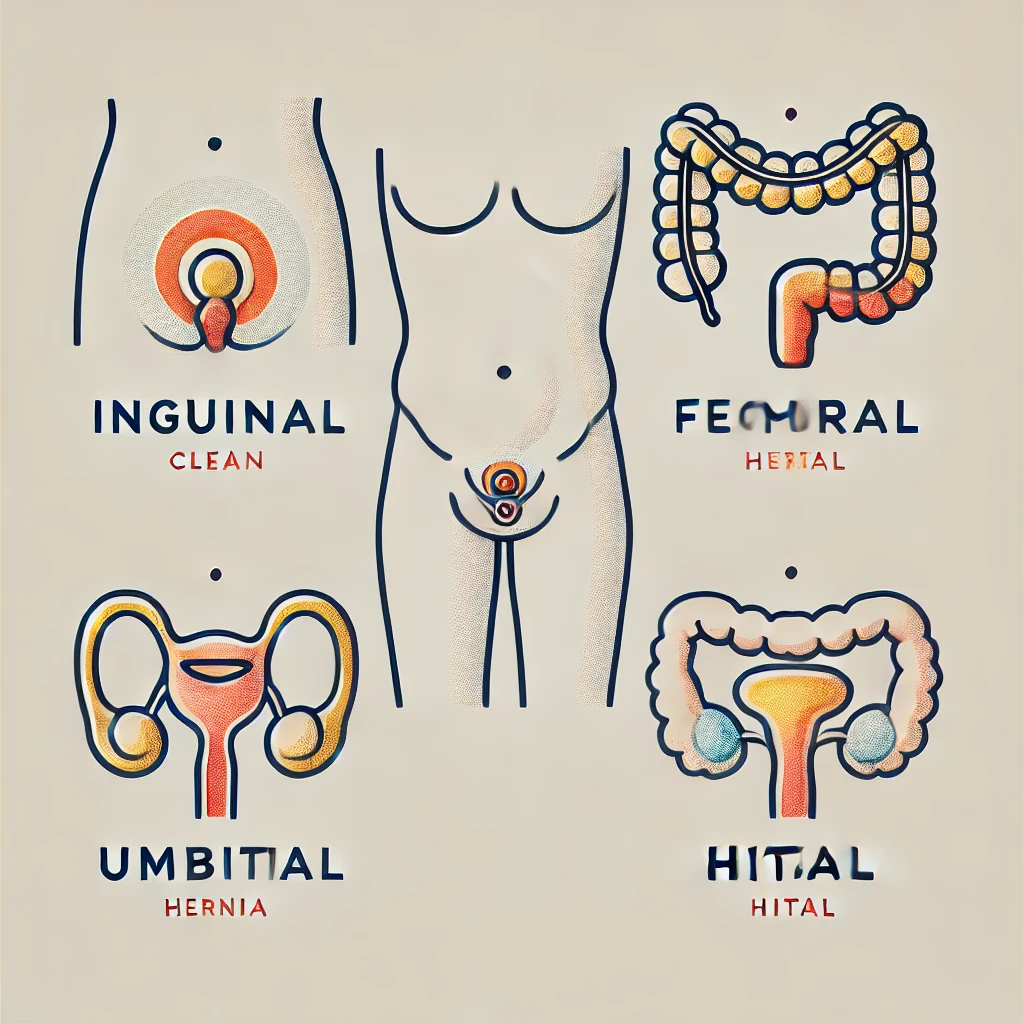
Hernias are classified based on location and clinical behavior.
(A) By Location
| Type | Location & Features |
|---|---|
| Inguinal Hernia | Groin region, most common type. Divided into direct and indirect. |
| Femoral Hernia | Below the inguinal ligament, higher risk of strangulation. |
| Umbilical Hernia | At the umbilicus, often congenital. |
| Incisional Hernia | Occurs at a previous surgical incision site. |
| Epigastric Hernia | Occurs in the midline above the umbilicus. |
| Hiatal Hernia | Protrusion of stomach into the thorax through the diaphragm. |
(B) By Clinical Behavior
| Type | Description |
|---|---|
| Reducible | Contents return to their normal position spontaneously or with manual pressure. |
| Irreducible/Incarcerated | Contents cannot be pushed back, often causing pain. |
| Strangulated | Blood supply is compromised, leading to ischemia—surgical emergency. |
3. Inguinal Hernia: High-Yield Focus
Inguinal hernias are the most common type and occur above the inguinal ligament.
| Type | Anatomical Defect | Relation to Inferior Epigastric Artery | Common in |
|---|---|---|---|
| Indirect Inguinal Hernia | Persistent patent processus vaginalis | Lateral to the artery | Young males, congenital |
| Direct Inguinal Hernia | Weakness in Hesselbach’s triangle | Medial to the artery | Older males, acquired |
Hesselbach’s Triangle (Direct Hernia Zone)
- Medial border: Rectus abdominis
- Inferior border: Inguinal ligament
- Lateral border: Inferior epigastric artery
4. Clinical Features of Hernias
| Feature | Findings |
|---|---|
| Pain & Swelling | Lump at the hernia site, may be reducible or irreducible. |
| Cough Impulse | Lump increases on coughing or straining. |
| Bowel Obstruction | In strangulated/incarcerated hernias (vomiting, distension). |
| Skin Changes | In strangulation (redness, tenderness, necrosis). |
5. Diagnosis & Investigations
(A) Clinical Examination
- Inspection: Location, size, cough impulse.
- Palpation: Determine reducibility, tenderness, and relation to inguinal ligament.
- Auscultation: Bowel sounds (present in hernia with intestinal contents).
(B) Imaging
| Test | Indication |
|---|---|
| Ultrasound | First-line for differentiating hernias from other groin masses. |
| CT Scan | Useful for complex or recurrent hernias. |
| MRI | Used in cases with suspected occult hernias. |
6. Management Strategies
(A) Conservative Management
- Observation for small, asymptomatic hernias.
- Trusses/binders in patients unfit for surgery.
(B) Surgical Management
| Surgical Approach | Indication |
|---|---|
| Open Hernia Repair (Lichtenstein technique) | Standard approach, using mesh reinforcement. |
| Laparoscopic Repair (TAPP/TEP) | Minimally invasive, preferred in bilateral or recurrent hernias. |
| Emergency Surgery | Strangulated or incarcerated hernias. |
7. Complications of Untreated Hernias
🚨 Strangulation → Ischemia → Necrosis → Perforation → Sepsis
🚨 Obstruction → Bowel dysfunction (vomiting, distension, absent flatus/stool)
🚨 Recurrence → Often due to inadequate repair or high intra-abdominal pressure
8. Key Takeaways
✅ Inguinal hernias are the most common type, classified as direct (medial) or indirect (lateral).
✅ Femoral hernias have a high risk of strangulation and require early surgical intervention.
✅ Strangulated hernias are surgical emergencies due to ischemic risk.
✅ Surgical repair is recommended for symptomatic or high-risk hernias.
Further Reading
- NHS Overview on Hernias: NHS UK
- NICE Guidelines on Hernia Repair: NICE Guidelines
Would you like additional case studies or diagnostic flowcharts for rapid clinical assessment? 🚀