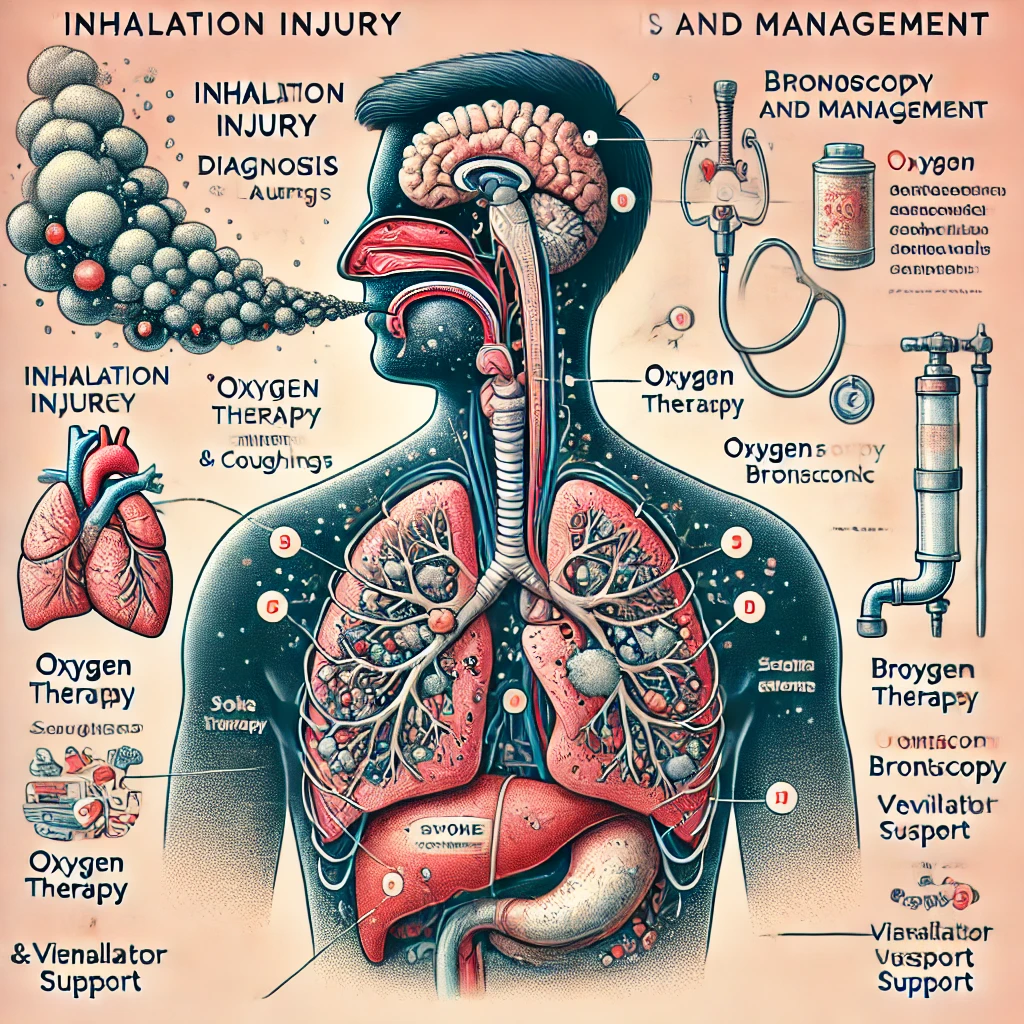
Inhalation injury occurs due to the inhalation of smoke, toxic gases, or superheated air, leading to airway inflammation, respiratory distress, and systemic toxicity. It is commonly seen in burn victims, house fires, and industrial accidents. Early recognition and management are critical to prevent respiratory failure and carbon monoxide or cyanide poisoning.
Pathophysiology
Inhalation injuries can affect three key areas:
- Upper Airway (Supraglottic Injury): Thermal injury causes edema, leading to airway obstruction.
- Lower Airway (Infraglottic Injury): Chemical irritation from smoke causes bronchospasm, alveolar damage, and inflammation.
- Systemic Toxicity: Carbon monoxide (CO) and cyanide poisoning impair oxygen delivery and cellular respiration.
Clinical Features (High-Yield for PLAB 1)
1. Early Signs (Suggesting Inhalation Injury)
- Facial burns with singed nasal hairs.
- Soot in the mouth/nose (Black sputum).
- Hoarseness, stridor, or difficulty speaking.
- Cough and wheezing.
- Carbonaceous sputum production.
- Progressive respiratory distress (Tachypnea, accessory muscle use).
2. Signs of Impending Airway Obstruction
- Stridor, difficulty breathing, or altered mental status, indicating the need for early intubation.
3. Systemic Toxicity Features
- Carbon monoxide poisoning: Confusion, dizziness, headache, cherry-red skin.
- Cyanide poisoning: Metabolic acidosis, hypotension, seizures, almond-scented breath.
More details on carbon monoxide poisoning: NICE Carbon Monoxide Poisoning Guidelines.
Diagnosis
1. Clinical Assessment (ABCDE Approach)
- Airway: Look for signs of obstruction (stridor, hoarseness).
- Breathing: Assess respiratory rate, use of accessory muscles, auscultation.
- Circulation: Monitor BP, HR, and signs of systemic toxicity.
2. Investigations
- Arterial Blood Gas (ABG):
- COHb levels: Carbon monoxide poisoning if COHb >10% (non-smokers) or >15% (smokers).
- Lactate >8 mmol/L: Suggests cyanide poisoning.
- Metabolic acidosis with normal PaO₂: Cyanide toxicity.
- Chest X-ray (CXR): Often normal initially but useful for detecting smoke inhalation lung injury.
- Bronchoscopy: To assess for airway burns and edema.
- Carboxyhemoglobin levels: To confirm carbon monoxide poisoning.
- Cyanide levels: If suspected systemic toxicity.
More on inhalation injury evaluation: UK Resuscitation Council: Smoke Inhalation Guidelines.
Management (High-Yield PLAB 1 Approach)
1. Airway Management
- Early intubation if:
- Stridor or hoarseness.
- Airway swelling.
- Decreased consciousness (GCS < 8).
2. Oxygen Therapy
- 100% Oxygen via Non-Rebreather Mask (Reduces COHb half-life from 4-6 hours to 90 minutes).
- Hyperbaric Oxygen (HBO) Therapy for severe carbon monoxide poisoning:
- COHb > 25%.
- Neurological symptoms (confusion, loss of consciousness).
- Severe metabolic acidosis.
- Pregnant patients with COHb > 15%.
3. Cyanide Poisoning Treatment
- Hydroxocobalamin (Vitamin B12a) – First-line antidote.
- Sodium thiosulfate – Alternative therapy.
- Sodium nitrite – Used in some protocols but can worsen methemoglobinemia.
More on cyanide poisoning management: BNF Cyanide Antidotes.
4. Supportive Care
- IV Fluids for hemodynamic support.
- Nebulized bronchodilators for bronchospasm.
- Analgesia (IV opioids) for burn-related pain.
- Steroids NOT recommended routinely (no proven benefit).
- Chest physiotherapy for airway clearance.
- Monitor for ARDS (Acute Respiratory Distress Syndrome).
Complications
- Acute respiratory failure.
- Pulmonary edema or ARDS.
- Carbon monoxide and cyanide poisoning.
- Bronchopneumonia (secondary infection).
- Neurological damage (due to hypoxia/toxicity).
Key Takeaways for PLAB 1
- Early intubation if airway compromise is suspected.
- 100% Oxygen therapy is the mainstay of treatment.
- Check COHb levels for carbon monoxide poisoning.
- Hydroxocobalamin is the antidote for cyanide poisoning.
- Monitor for delayed pulmonary complications (ARDS, pneumonia).
For further reading: