Prior to surgery, it is crucial to stop certain medications, foods, and drinks to reduce the risk of complications such as bleeding, delayed gastric emptying, and anesthetic interactions. This guide outlines best practices based on UK guidelines (NICE, Royal College of Anaesthetists, and British National Formulary – BNF).
1. Medications to Stop Before Surgery
A. Anticoagulants & Antiplatelets
| Medication | When to Stop | Considerations/Alternatives |
|---|---|---|
| Warfarin | 5 days before | Bridge with LMWH if high thrombotic risk |
| DOACs (Apixaban, Rivaroxaban, Edoxaban, Dabigatran) | 24-48 hours before (longer in renal impairment) | Bridging not required in most cases |
| Clopidogrel, Ticagrelor | 5-7 days before | Continue if recent stent (<6 months); consult cardiologist |
| Aspirin | Continue in most cases | Stop 7 days before if high bleeding risk |
| Low Molecular Weight Heparin (LMWH) | Stop 24 hours before | Prophylactic doses may be continued |
B. Antihypertensives
| Medication | When to Stop | Considerations |
|---|---|---|
| ACE inhibitors (Ramipril, Lisinopril) | On the day of surgery | Risk of intraoperative hypotension |
| ARBs (Losartan, Valsartan) | On the day of surgery | Monitor blood pressure closely |
| Beta-blockers (Bisoprolol, Atenolol) | Continue | Stopping can cause rebound hypertension |
| Calcium channel blockers | Continue | No major perioperative concerns |
| Diuretics (Furosemide, Spironolactone) | Stop on the day of surgery | Risk of hypovolemia |
C. Diabetes Medications
| Medication | When to Stop | Considerations |
|---|---|---|
| Metformin | 24-48 hours before major surgery | Risk of lactic acidosis |
| SGLT2 Inhibitors (Empagliflozin, Dapagliflozin) | 3 days before | Risk of ketoacidosis |
| Insulin | Adjust dose | Long-acting insulin usually continued with dose reduction |
| Sulfonylureas (Gliclazide, Glibenclamide) | Stop on the day of surgery | Risk of hypoglycemia |
D. Other Medications
| Medication | When to Stop | Considerations |
|---|---|---|
| NSAIDs (Ibuprofen, Naproxen) | 48 hours before | Increased bleeding risk |
| Methotrexate | Hold for 1 week before major surgery | Risk of immunosuppression |
| Hormone Replacement Therapy (HRT) | 4 weeks before major surgery | Increased VTE risk |
| Oral Contraceptives | 4 weeks before major surgery | Consider temporary switch to alternative contraception |
| Monoamine Oxidase Inhibitors (MAOIs) | 2 weeks before | Risk of hypertensive crisis with anesthesia |
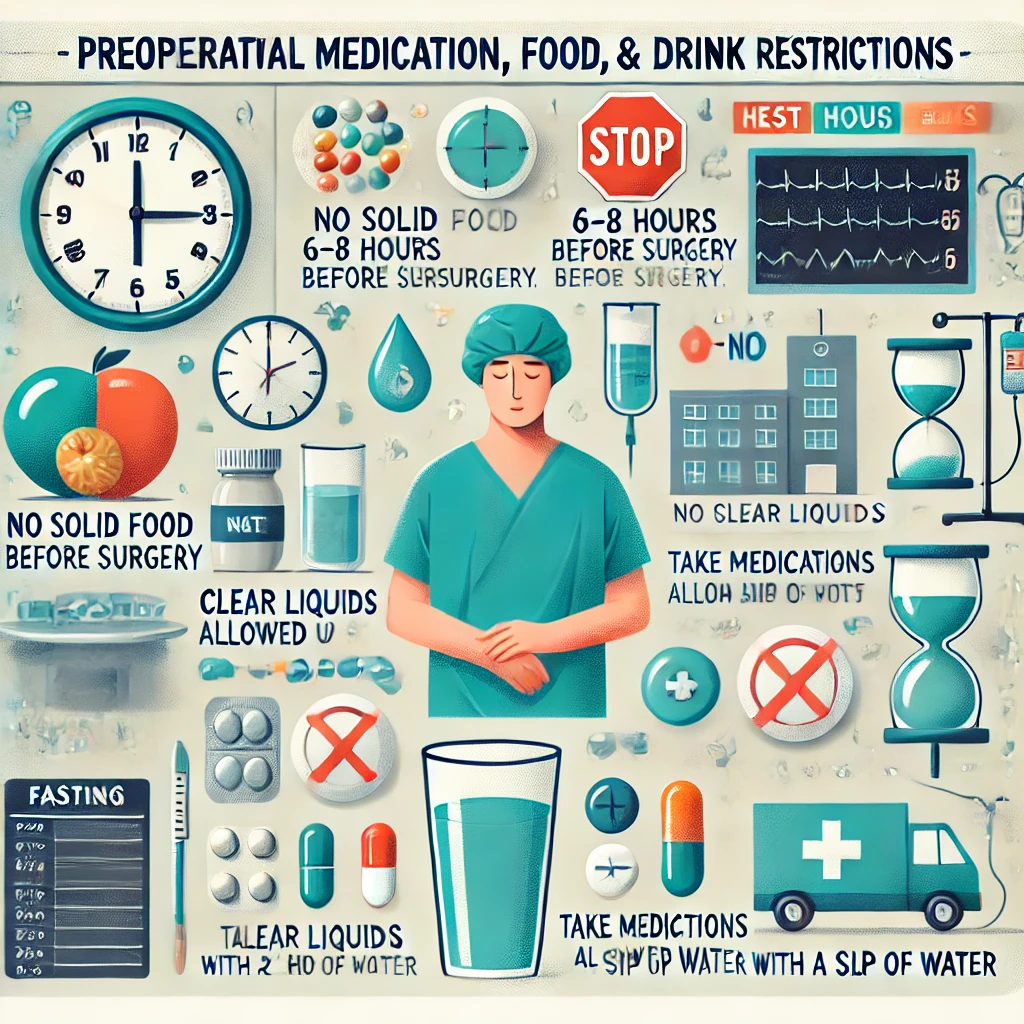
2. Food and Drink Restrictions Before Surgery
A. General Fasting Guidelines (NICE & Royal College of Anaesthetists)
- Solid food: Stop 6 hours before surgery.
- Clear fluids (water, black tea, black coffee, diluted juice): Stop 2 hours before surgery.
- Milk, Alcohol, and Carbonated Drinks: Stop 6 hours before surgery.
B. Special Dietary Considerations
- Patients with diabetes: Require an individualized fasting plan.
- Gastroesophageal reflux disease (GORD): May require earlier cessation of fluids.
- Patients on enteral feeds: Usually stopped 6 hours before surgery.
3. Summary of Key Recommendations
✅ Stop anticoagulants and antiplatelets based on thrombotic vs bleeding risk. ✅ Hold antihypertensives selectively to prevent intraoperative hypotension. ✅ Adjust diabetes medications to avoid hypoglycemia and ketoacidosis. ✅ Stop NSAIDs, HRT, and contraceptives preoperatively to reduce bleeding and clot risks. ✅ Follow strict fasting protocols to prevent aspiration during anesthesia.
Conclusion
Preoperative medication, food, and drink restrictions play a critical role in optimizing surgical outcomes and preventing complications. Following UK guidelines ensures patient safety while balancing bleeding, clotting, and metabolic risks. Always consult with the surgical and anesthetic team for case-specific recommendations.